Abstract
Background: The initial diagnosis of acute myeloid leukemia (AML) and time-points when a change in treatment is needed can be very overwhelming periods for patients and providers. Clinicians are gathering and synthesizing data, including patient symptoms and clinical status, laboratory abnormalities and pathology details, along with cytogenetic and molecular information, to devise an appropriate treatment plan for the patient. Patients and their care partners are absorbing a significant amount of information, all while facing a life-changing diagnosis or the distressing burden of deciding on or acclimating to a new treatment. Some questions may remain unasked in a time-constrained office visit, both that the patient wishes to ask or that the provider would wish to ask but needs to prioritize other topics. An electronic platform may allow the patient to communicate additional important information that may influence their care, while not relying on the clinical team to gather these data. In addition, there are few studies that focus on patient beliefs, goals, preferences, and top concerns at time of treatment decision making.
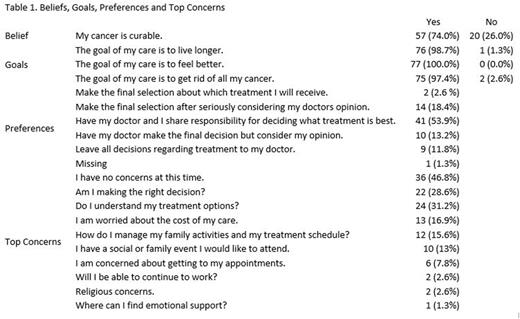
Methods: Patients with a diagnosis of AML and at a treatment decision making visit were recruited from three academic cancer centers. Prior to seeing the physician, each patient used an electronic tablet to complete baseline surveys that included beliefs about curability of their cancer, goals of care, decision making preferences, top concerns, and a modified geriatric assessment (mGA) screening tool. The mGA includes four domains: age, activities of daily living (ADLs), instrumental ADLs, and comorbidities. mGA survey results along with history of falls was used to create the Frailty Index (FI). All questionnaire results were immediately displayed on a dashboard for the physician to refer to during the clinical visit.
Results: 77 patients were enrolled in the study. Median age was 71 years (range:61-88). 50 were female (64.9%), 67 white (87.0%), and 33 college educated (42.9%). 43 (56.6%) were former or current smokers. 52 (72.7%) were interested in clinical trial participation. 50 (64.9%) did not have an advanced directive. FI results for 76 patients were 28 (36.8%) fit, 25 (32.9%) intermediate fit, and 23 (30.3%) frail. One patient did not complete the mGA. At baseline, 57 (74%) believed their cancer was curable. 76 (98.7%) agreed a goal of care was to live longer, 77 (100.0%) agreed a goal was to feel better, and 75 (97.4%) agreed a goal was to get rid of all of the cancer. 41 (53.9%) wanted to share responsibility for deciding what treatment was best with their physician, while 16 (21.0%) wanted to make the final selection and 19 (25.0%) wanted to leave decisions regarding treatment to their physician. 1 (1.3%) patient response was missing. Patients selected up to 5 responses from a list of common concerns. Although 36 (46.8%) indicated they had no concerns at the time, 24 (32.2%) selected "Do I understand my treatment options?", 22 (28.6%) selected "Am I making the right treatment decision?", 13 (16.9%) selected "I am worried about the costs of my care", 12 (15.6%) selected "How do I manage my family activities and my treatment schedule. 8 (29.6%) patients received intensive therapy, 15 (55.6%) non-intensive therapy and 4 (14.8%) clinical trial. Patients were able to complete the surveys unassisted in an average time of 16.24 minutes and providers reported an average of 3.5 minutes to review the dashboard. At three months, 52 (68.0%) study participants were alive, 21 (28.0%) were deceased and 4 (5.0%) were lost to follow up.
Discussion: Although most would agree including the patients goals, beliefs, preferences, and top concerns in the treatment decision discussion, a systematic approach to eliciting and documenting the information is often missing in the hectic clinic workflow. This study showed that use of an electronic tablet-based process to allow consistent data collection and immediately present the responses on a dashboard facilitates the inclusion of important patient information while not impeding workflow. These results also provide insight into patient perception of outcomes in AML, common concerns prior to starting treatment and shared-decision making. Identifying patients goals, beliefs, decision making preferences, and top concerns can provide physicians with an opportunity to individualize treatment plan for patients with AML.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal